Hi everyone! I am currently in one of the most obscure fields of radiology known as nuclear medicine. The goal of nuclear medicine is to treat and diagnose diseases based on cellular function and physiology, as opposed to waiting for changes in the physical features of tissue to diagnose conditions. This is advantageous because potentially life threatening conditions can be identified in very early stages.
The main tools that nuclear medicine uses are radiopharmaceuticals. Radiopharmaceuticals are formed from chemically bonding radionuclides (which are essentially radioactive materials) and pharmaceutical compounds. Once formed, radiopharmaceudicals (which typically emit gamma radiation) target specific tissues in the body and then images of the target tissues are captured using a gamma camera in a form of diagnostic imaging known as scintigraphy. A gamma camera can be thought of as a much more sophisticated pinhole camera, because the captured images are essentially pixelated by gamma of radiation. The reason that gamma radiation is used instead of alpha or beta radiation is that gamma radiation has a much larger frequency and will penetrate through tissue much more easily, thus creating a better image.
 |
| Ventilation/Perfusion Scan |
The above image is a ventilation/perfusion scan and is an example of why nuclear medicine is oftenly referred to as "unclear" medicine. Every image in nuclear medicine looks this unclear, however it is at least obvious that these are lungs. Despite how old fashioned this image looks, it can be used by a nuclear radiologist to check for a pulmonary embolism - a condition that can be fatal if untreated.
 |
| Bone Scintigraphy |
The above image is a bone scintigraphy/scan. The scan has the same underlying idea as the other scans in nuclear medicine, except the pharmaceutical that is bonded to the radionuclide (typically technetium-99m) targets the bones. This scan checks for bone abnormalities. The idea is that the parts of the bones that are more active will have a higher amount of blood flow and absorb more of the radiopharmaceutical and show up as "dark spots" on the scan. The dark spots can simply be from fractured bones trying to heal themselves, but they could also be from cancers on the bone. For example, prostate cancer tends to spread to the spine and breast cancer tends to spread to the ribs. I am no doctor, but this guy looks like he is in bad shape. An important detail to note here is that nuclear medicine does not diagnose what type of cancer a person has, but rather that there could be cancer. For example, some people have naturally occurring symmetrical dark spots on bone scans that are not cancerous.
 |
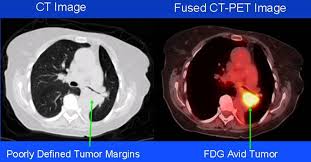
| CT-PET Image |
Another powerful tool available to nuclear radiologists is a PET-CT Scanner. A lone CT or PET scan may be difficult to read and a doctor may overlook a small detail, but together a CT-PET scan is truly a guide to the human body. The PET scan uses radioactive glucose to measure metabolic activity (the idea being that overactive and possibly cancerous cells will be metabolically over active) of tissues in the body, while the CT scan acts a map to determine where exactly a possibly cancerous tumor may be. It is important to note that once again, nuclear medicine does not determine if a growth is truly cancerous, but rather that something could be cancerous. For example, a PET scan simply measures metabolic activity through the use of radioactive glucose. These tissues that are metabolically overactive will show up as brighter and as a "hot spot" on a PET scan, however something that is a "hot spot" on the PET-CT scan could be due to an injury or overactive lymph node as easily as it could be cancerous. The ability to distinguish between "suspicious" and "non-suspicious" hot spots on PET-CT scans comes form both an expensive knowledge of physiology and experience - which is one reason why experienced attending Nuclear Radiologists make "the big bucks." Last week, there was a patient that had a history of fungal infections and the attending nuclear radiologist was unable to determine if a nodule in the lungs was due to an infection or cancer.
The above images are PET-CT scans of the lungs, and both scans display a pulmonary nodule as a very bright hot spot.


